Conditions
Several conditions can lead to or worsen back, leg, and neck pain.
Click on the condition below to learn more about it.
Adjacent Segment Disease
Overview
Adjacent Segment Disease (ASD) is a degenerative disc disease (DDD) that can result from stress on a level adjacent to a former spinal fusion procedure or can be attributed to the natural progression of DDD involving additional levels of the spine. This can lead to:
- Disc bulging or disc herniation
- Bone spurs or osteophytes
- Loss of disc space or alignment
- Nerve impingement
This can result in pain at the levels adjacent to the previous fusion.
Cervical Disc Degeneration
Overview
Degeneration of the cervical disc occurs as we age. Injury, daily wear and tear, and genetics also contribute to this process. Degeneration consists of damage to the cervical disc, which may then become narrowed or may herniate. This causes symptoms of pain, numbness, tingling, and/or weakness in the arms or shoulders, and may also cause neck pain. The available treatments are directed at these symptoms and do not represent a cure for the degenerative process.
Symptoms
- Neck pain
- Pain, numbness, or tingling in the arms or shoulders
- Weakness in the arms or shoulders
Degenerative Scoliosis
Overview
Adult degenerative scoliosis is a condition where a right-left or lateral curve develops in a previously straight spine secondary to advanced degenerative disc disease. This curvature occurs as a result of deterioration (or degeneration) of the disc space and joints in the back of the spine. As the joints degenerate they create a misalignment in the back, resulting in a bend or curvature. This misalignment of the spine can cause back and/or leg pain due to muscle fatigue and nerve impingement and may lead to a condition known as lumbar (lower back) stenosis. Adult degenerative scoliosis is more common in the lower back and most frequently occurs in people over 65 years of age.
Symptoms
- Pain in the back and/or legs
- Spinal deformity
- Pain may occur on one or both sides
- Pain that worsens when standing or walking
- Lying down relieves pressure on the spine and reduces pain
- Uneven shoulders or waist
- Shoulder blade protrusion
Diagnosing Adult Degenerative Scoliosis
Your doctor will perform a physical examination to identify areas of pain and weakness and will evaluate your balance and the overall movement of your spine. Your doctor will also collect information about the history of your symptoms, including medicine you have taken for your condition. After your examination, your doctor may use tests to help establish his or her diagnosis. Some of these tests include X-ray, CT (computed tomography) scan, and MRI (magnetic resonance imaging). Together, all of these techniques help to confirm a diagnosis of adult degenerative scoliosis.
Degenerative Spondylolisthesis
Overview
Spondylolisthesis (spon-di-loh-lis-thee-sis) is a condition where one vertebra has slipped forward over another one below it. This misalignment typically occurs as a result of advanced degenerative disc disease, stress fractures, or congenital abnormalities, and in rare cases from a tumor or trauma. Degenerative spondylolisthesis is a consequence of the aging process in which the bones, joints, and ligaments in the spine grow weakened and become less able to maintain the alignment of the spinal column. This type of spondylolisthesis typically occurs at one of two levels in the lumbar spine:
- L4-L5 (most common)
- L3-L4
Degenerative spondylolisthesis is more common in people over age 50 and, in particular, among individuals over age 65. Women are two to three times as likely as men to be diagnosed. Spondylolisthesis can cause impingement of the nerves and/or fatigue of the back muscles and may result in lower back and/or leg pain.
Symptoms
- Lower back and/or leg pain
- Sciatica, an aching pain in the hips, buttocks, and lower back that radiates (spreads) into the back of the thighs and legs
- A shuffling gait when walking
- Weakness in the lower extremities
- Abnormal posture
Diagnosing Spondylolisthesis
Your doctor will perform a physical examination to identify areas of pain and weakness and will evaluate your balance and the overall movement of your spine. Your doctor will also collect information about the history of your symptoms, including medicine you have taken for your condition. After your examination, your doctor may use tests to help establish his or her diagnosis. Some of these tests may include X-ray, CT (computed tomography) scan, and MRI (magnetic resonance imaging). Together, all of these techniques may help to confirm a diagnosis of spondylolisthesis.
Herniated disc
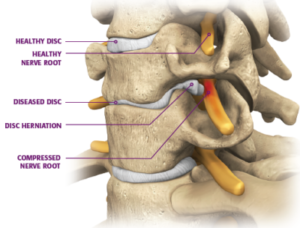
What is a herniated disc?
When the gelatinous center of the intervertebral disc pushes out through a tear in the fibrous wall, the disc herniates. This disc herniation adds pressure to the surrounding spinal nerves causing mild to severe pain. It is one of the most common spinal disorders.
What causes herniated discs?
Herniated discs may be caused by simple wear and tear from repeated movement over time or disc degeneration. During the natural aging process, spinal discs lose some of their water content making it difficult to support the load from above vertebrae.
Other causes of a herniated disc may include the following:
- Long standing trauma
- Hereditary or congenital abnormalities
- Stress fractures
- A sudden heavy strain or increased pressure
What are the symptoms?
While a herniated disc can happen at any level of the spine, it most commonly occurs in the lumbar region or lower back.
Symptoms of a herniated disc may include:
- Pain at the site
- Pain, numbness, weakness, or tingling in the arms or legs
- Pain that worsens when bending, twisting, and/or sitting
- Muscle spasms
In addition to these symptoms, if the herniated disc is located in the cervical spine or neck, symptoms may include:
- Loss of bladder control
- Loss of coordination
- The feeling of heavy limbs
- Trouble balancing
If you feel that you are experiencing any of these symptoms, please consider seeing a physician for an accurate diagnosis.
What are the treatment options?
If a herniated disc is established as the diagnosis, your doctor may recommend one or more of the following treatment plans based on your specific condition:
- Physical therapy and strengthening exercises
- Rest and restriction of physical activity
- Injections (corticosteroids) to help reduce the pain and swelling
- Medications and analgesics to reduce pain and swelling (typical medications include non-steroidal anti-inflammatory drugs, or NSAIDs)
- Application of heat and/or ice to help reduce pain, inflammation, and muscle spasms
If your symptoms do not improve with other methods and back pain continues to diminish your quality of life, your physician may suggest spinal surgery. Surgical solutions for a herniated disc may include the following:
- Discectomy
- Laminectomy
Lumbar Degenerative Disc Disease
Overview
Lumbar degenerative disc disease (DDD) is defined simply as the wear and tear of the intervertebral disc, which may result from normal aging or be due to longstanding trauma. It involves small tears in the annulus of the disc (elastic outer ring of collagen fibers) and lack of water content of the nucleus of the disc (soft gel center). The degenerative cascade can lead to disc bulging, development of bone spurs (or osteophytes), and loss of disc space height and/or alignment, which can cause nerve impingement. DDD can also lead to degenerative instability, the loss of the ability of the spine under physiologic loads to maintain its pattern of normal movement due to disc degeneration.
Symptoms
- Pain at the site of the injury
- Pain, numbness, or tingling in the legs
- Strong pain that tends to come and go
- Pain is worse when bending, twisting, and/or sitting
- Lying down relieves pressure on the spine
Diagnosing Degenerative Disc Disease
Your doctor will perform a physical examination to identify areas of pain and weakness and will evaluate your balance and the overall movement of your spine. Your doctor will also collect information about the history of your symptoms, including medicine you have taken for your condition. After your examination, your doctor may use tests to help establish his or her diagnosis. Some of these tests include X-ray, CT (computed tomography) scan, and MRI (magnetic resonance imaging). Together, all of these techniques help to confirm a diagnosis of lumbar DDD.
Lumbar Spinal Stenosis
Overview
Degenerative or age-related changes in our bodies can lead to compression of the nerves (pressure on the nerves that may cause pain and/or damage). Lumbar spinal stenosis is a gradual narrowing of the space where nerves pass through the spine, and may be a result of aging and wear and tear on the spine from everyday activities (i.e., degenerative disc disease) and/or resultant positional changes of the vertebrae.
Symptoms
- Decreased endurance during physical exercise and activities
- Weakness and/or loss of balance
- Numbness and a “prickly” feeling in your legs, calves, or buttocks
- Aching, dull back pain radiating (spreading) to your legs
- Symptoms improve when you sit, lean forward, lie on your back, or sit with your feet raised
- Neurogenic claudication
Diagnosing Lumbar Spinal Stenosis
Your doctor will perform a physical examination to identify areas of pain and weakness, and will evaluate your balance and the overall movement of your spine. Your doctor will also collect information about the history of your symptoms, including medicine you have taken for your condition. After your examination, your doctor may use tests to help establish his or her diagnosis. Some of these tests include X-ray, CT (computed tomography) scan, and MRI (magnetic resonance imaging). Together, all of these techniques help to confirm a diagnosis of lumbar spinal stenosis.
Myelopathy
Overview
Myelopathy is a symptom of an underlying spinal condition that compresses or irritates the spinal cord. When the spinal cord is injured, the body and brain cannot communicate with each other properly and this inefficiency can present as myelopathy. Symptoms can present as:
- The feeling of heavy limbs
- Difficulty balancing
- Muscle weakness
- Loss of coordination
- Loss of bladder/bowel control
Causes
Myelopathy is most commonly the result of:
- Degenerative disc disease
- Spinal stenosis
- Tumor
- Trauma
Consequences of these conditions include compression of the spinal cord through loss of normal spacing, osteophyte formation (bone spurs), and/or bulging or herniated discs.
If you feel that you are experiencing myelopathy, please consider seeing a physician for an accurate diagnosis.
Radiculopathy
Overview
Radiculopathy is a symptom of an underlying spinal condition that compresses or irritates spinal nerves. It can present as pain, numbness, tingling, or weakness along the path of a nerve.
For example, if a spinal nerve in the lumbar region is irritated, radiating pain may be experienced along the associated nerve route that begins in the lower back and travels through the leg.
Causes
Radiculopathy is most commonly the result of a condition affecting an intervertebral disc, such as a bulging or herniated disc that presses against the spinal nerves. Other causes may include:
- Degenerative disc disease (DDD)
- Spinal stenosis
- Bone spurs
- Tumor
- Trauma
- Diabetes
If you feel that you are experiencing pain radiating from your back to your limbs, please consider seeing a physician for an accurate diagnosis.
